Identify hypogonadism with our testing strategy
Male hypogonadism is a clinical syndrome resulting from decreased testosterone and/or sperm production.1 It is estimated that 35% of men over 45 years of age have hypogonadism.2 There is a higher prevalence of hypogonadism in older men, obese men, and men with type 2 diabetes.2
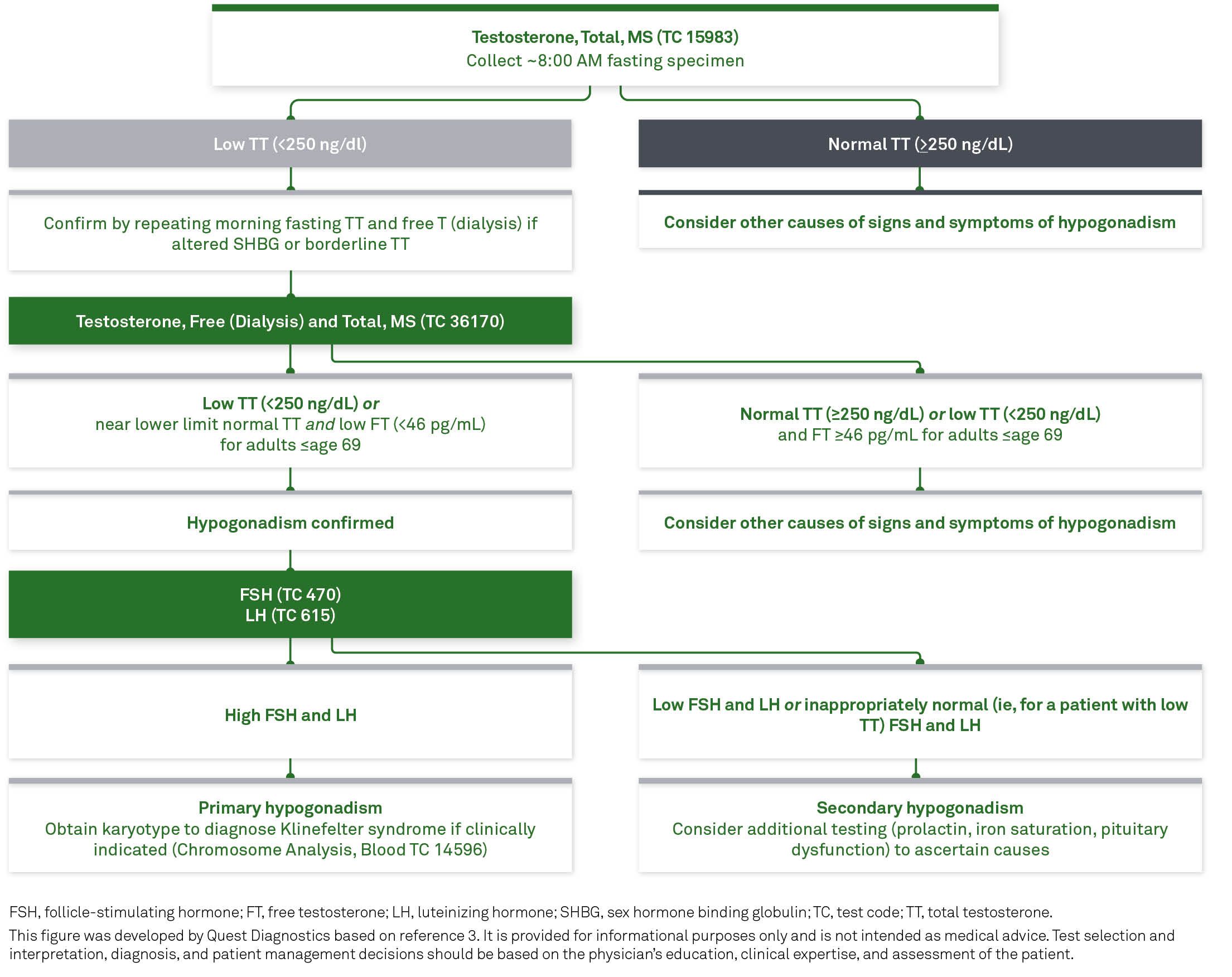
Hypogonadism can occur in 3 forms: primary, secondary, and combined. If initial and confirmatory testing indicates low testosterone, follicle stimulating hormone (FSH), and luteinizing hormone (LH) should be measured to distinguish between primary and secondary hypogonadism.1
When hypogonadism is diagnosed in men, additional diagnostic evaluation is recommended to determine the cause(s), which are classified as either organic or functional.
Organic causes include congenital, structural, or destructive disorders that suppress the hypothalamus, pituitary, or testis. Functional causes include conditions that suppress gonadotropins and testosterone concentrations, including diabetes, obesity, and the use of opioids.1
Laboratory testing is recommended for the diagnosis of men with suspected hypogonadism, especially when conditions associated with a high prevalence of low testosterone are present.1,3
| Specific |
Suggestive | Nonspecific |
| Incomplete or delayed sexual developmenta Loss of body hair Very small testes (<6 mL) |
Reduced libidoa Decreased spontaneous erections |
Decreased energy, motivation, initiative, self-confidence Increased body fat, BMI |
| Conditions associated with decreased SHBG1 |
| Insulin resistance |
| Obesity |
| Diabetes mellitus |
| Use of glucorticoids, some progestins, and androgenic steroids |
| Nephrotic syndrome |
| Hypothyroidsim |
| Acromegaly |
| Polymorphisms in the SHBG gene |
| Conditions associated with increased SHBG1 |
| Aging |
| HIV disease |
| Cirrhosis and hepatitis |
| Hyperthyroidism |
| Use of some anticonvulsants |
| Use of estrogens |
| Polymorphisms in the SHBG gene |
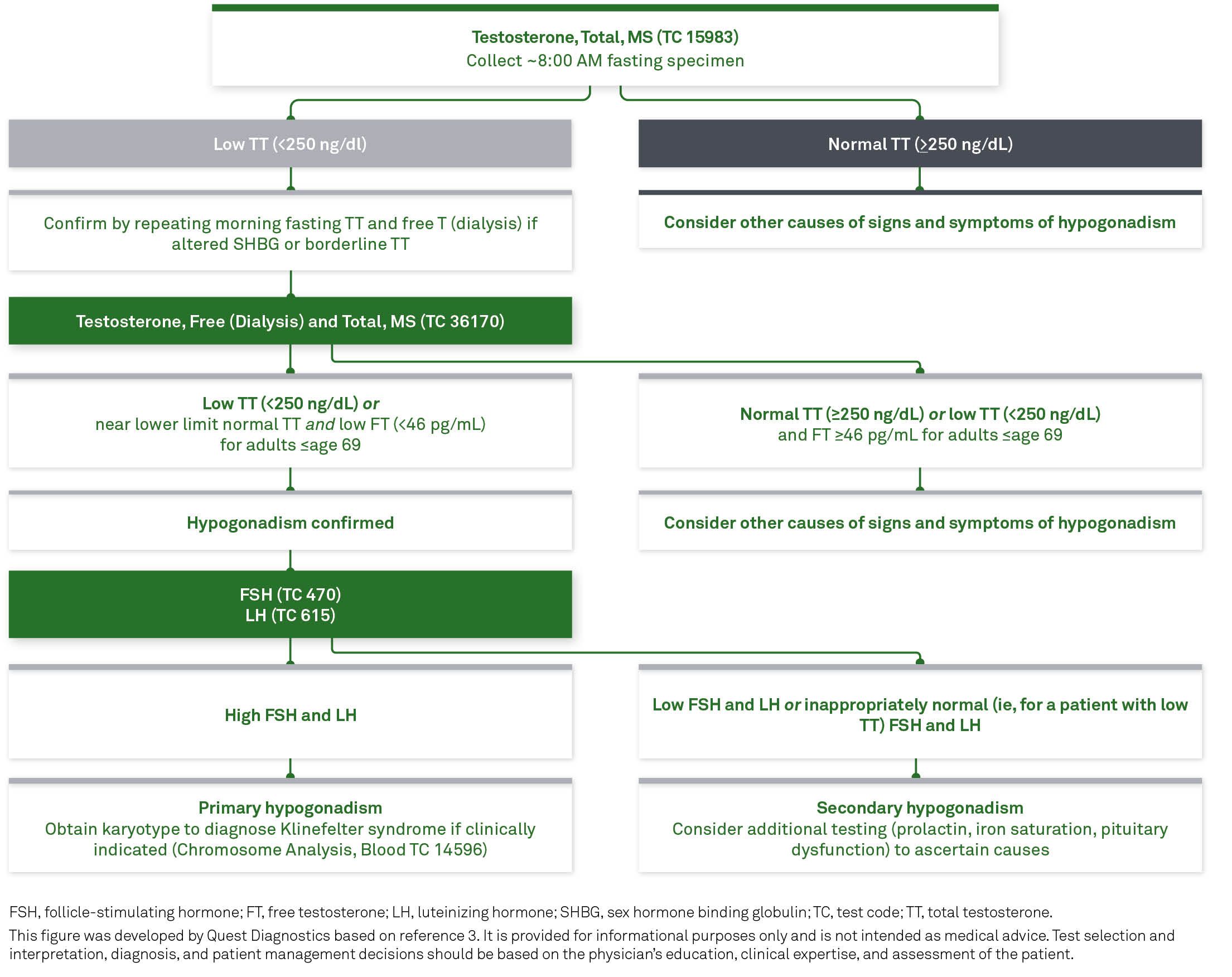
Initial diagnostic testing for low testosterone involves measuring morning fasting total testosterone (TT)1 by Liquid Chromatography, tandem mass spectrometry (LC-MS/MS), which is advantageous because:
Quest Diagnostics offers a Total Testosterone LC-MS/MS assay that is certified by the CDC Laboratory/Manufacturer Hormone Standardization (HoSt) Program, which is the Endocrine Society–recommended assay for healthy men older than age 18.1,4
Measurement of free testosterone (FT) is guideline-indicated if TT is reported near the lower limit of normal or if alterations in SHBG that affect TT are suspected.1 Guidelines recommend measuring FT by LC-MS/MS and an equilibrium dialysis method.1 The Endocrine Society recommends to confirm a low testosterone value with a second 8 AM measurement, and to initiate early treatment if both values are below normal.
The Endocrine Society recommends:
Quest Diagnostics offers several tests to help you monitor patients undergoing testosterone therapy, including:
Explore the common symptoms of hypogonadism, guideline-recommended testing options to help inform a diagnosis, and recommended testing options for patients on testosterone therapy.

References
Connect with our experts to help you manage the care pathway for patients with testerone deficiency.